Dual Diagnosis Treatment
in Orange County

What is Dual-Diagnosis Treatment?
Be Brave. Get Help.
Dual Diagnosis
20% of American adults have some form of mental illness
Mental health conditions can cause changes in thought, emotion and behavior and interfere with healthy social functioning. Mental illnesses negatively impact mood, health and sense of wellbeing. They can cause problems with relationships, employment and other life domains.
The most common mental illnesses are anxiety and depression. According to the American Psychiatric Association, around 40 million Americans suffer from an anxiety disorder in any given year, and 14.8 million live with major depression. All told, nearly 20 percent of all American adults have some form of mental illness at any given time.
Mental illness is a medical condition involving the brain, and it’s treatable. The most common and successful treatments for mental illness are a combination of medicine and counseling. Medications balance neurotransmitters, or brain chemicals, that are involved in the illness. Counseling helps individuals cope with symptoms and change dysfunctional thought and behavior patterns that stem from–and contribute to–the mental illness.
Substance abuse, addiction, and dependence are all diagnosed under the umbrella of a substance use disorder, which is classified as mild, moderate, or severe, depending on how many diagnostic criteria you meet. But substance abuse, addiction, and dependence are not the same things.
Substance abuse is the act of using drugs or alcohol in a way that causes problems in your life, such as relationship, financial, legal or health problems. The most common form of substance abuse is binge drinking.
The Centers for Disease Control reports that one in six Americans -37.4 million people- binge drink around once a week, consuming around seven drinks during the binge.
Using any illegal drug, or using prescription drugs in a way other than exactly as prescribed, are forms of substance abuse because they put you at risk for legal troubles and can lead to dangerous situations.
Addiction may result from heavy substance abuse. If you’re addicted, you’ll continue to use drugs or alcohol despite the negative consequences. You may want to quit or try to stop, but find you can’t. Our substance abuse treatment in Orange County, CA, provides the support and guidance needed to break this cycle and begin a path to recovery.
Addiction is the result of physical and chemical brain changes that lead to compulsive drug-seeking and drug-using behaviors, driven by intense cravings caused by a re-wiring of the brain’s reward circuit.
Addiction almost always has underlying causes, such as chronic stress, a history of trauma, or a mental illness. It changes the way you think and behave, and it causes serious problems in your life.
Dependence is a physical reliance on drugs or alcohol marked by withdrawal symptoms that occur when you stop using. With heavy substance abuse, the brain changes its chemical function in order to compensate for the substance. For example, alcohol initially increases the activity of GABA, a neurotransmitter that causes feelings of calm and well-being. At the same time, it decreases the activity of glutamate, which is responsible for feelings of excitability. But heavy alcohol abuse causes the brain to compensate by reducing the activity of GABA and increasing the activity of glutamate.
As a result, tolerance develops, which means you need larger amounts of alcohol to get the desired effects. But as you drink more, the brain continues to compensate, and at some point, the chemical function of the brain may shift so that it now operates more comfortably when alcohol is present than when it’s not. Then, when you suddenly stop using the substance, normal chemical brain function rebounds, and this causes the onset of physical withdrawal symptoms.
Reach out to verify your insurance coverage for addiction treatment
Why Co-Occurring Disorders Are So Common
Dual diagnosis is very common. The National Alliance on Mental Illness points out that around one-third of people who have any type of mental illness, such as anxiety or depression, and half of those with a severe mental illness, such as schizophrenia or bipolar, also have a substance use disorder. 2 Additionally, around one-third of people who heavily abuse alcohol and more than half of people who abuse drugs also have a mental illness.
- Drug or alcohol abuse may cause a mental illness to develop, or it can worsen an existing mental illness. This is due to the chemical changes that occur in the brain with heavy substance abuse.
- People who have a mental illness are very likely to self-medicate with drugs or alcohol in an attempt to reduce the discomfort of the symptoms.
- Overlapping factors for both mental illness and substance abuse, such as stress and trauma, put some people at a higher risk of developing co-occurring disorders.
Dual Diagnosis Risk Factors
Overlapping Genetic Risks
A number of areas of the human genome play a role in the development of both substance use disorders and mental illnesses. Some genes have a direct influence, such as the way the body metabolizes drugs or alcohol. Other genes have an indirect influence, such as a tendency toward taking risks.
Involvement of Similar Brain Regions
Some brain regions are involved in both substance use disorders and mental illness. For example, the neurotransmitter dopamine, which is a major player in the reward circuit of the brain, plays a role in both addiction and depressive disorders.
Environmental Factors
Environmental factors, such as high stress or a dysfunctional family system, can influence both substance abuse and mental illnesses. For example, chronic stress can lead to an anxiety disorder, which can lead to self-medication with drugs or alcohol.
Mental Illnesses Commonly Cited in Dual Diagnosis
Anxiety disorders include generalized anxiety disorder, panic disorder and social anxiety disorder. These disorders produce a sense of doom and may cause sleep disturbances and feelings of restlessness. It’s common for people to use drugs or alcohol to reduce feelings of anxiety or to bring on sleep.
Depressive disorders include major depression and bipolar disorder. Depressive disorders are associated with feelings of sadness, hopelessness, and helplessness. People with depression may use drugs or alcohol in an attempt to feel positive emotions or numb the pain of negative emotions. Around half of all people with bipolar disorder have a lifetime history of a substance use disorder.
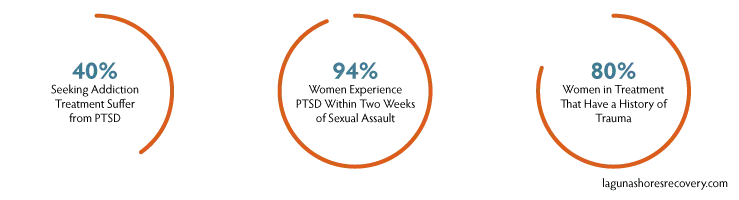
Post-traumatic stress disorder occurs as the result of trauma and includes symptoms like anger, fear, insomnia, flashbacks, and nightmares. According to one study, 40 percent of people seeking treatment for addiction suffer from PTSD. Another study found that more than half of combat veterans with PTSD eventually develop an addiction to alcohol.
According to the National Institutes on Health, sexual abuse is the most common cause of PTSD in women, with one study finding that 94 percent of women experience PTSD symptoms within two weeks of a sexual assault. A study in the journal Psychiatric Services found that up to 80 percent of women in treatment for addiction report a history of trauma, most commonly resulting from physical or sexual abuse.
Obsessive-compulsive disorder causes compulsive, repetitive thoughts and behaviors that can interfere with normal daily living. People with OCD may use drugs or alcohol to reduce intrusive symptoms. According to an article in the Journal of Anxiety Disorders, 27 percent of people with OCD also have a lifetime history of a substance use disorder.
Eating disorders, such as anorexia, bulimia or binge-eating disorder, often lead to drug or alcohol abuse as a way to control the appetite, reduce feelings of depression and cope with low self-esteem. Up to half of all people with an eating disorder abuse drugs or alcohol, according to an article in the journal Social Work.
While self-medication with drugs and alcohol is very common among people with a mental illness, drug and alcohol abuse almost always makes a mental illness worse, and it can even cause the onset of a mental illness that didn’t exist before.
How Co-Occurring Disorders are Diagnosed
It can be difficult to determine which came first–the substance use disorder or the co-occurring mental illness–since symptoms can overlap. But sorting out the symptoms and making an accurate diagnosis is essential for successfully treating co-occurring disorders.
This typically occurs during detox, which is the first step in treating a substance use disorder. During detox, a variety of assessments are used to identify an individual’s unique issues and needs. Assessments include a comprehensive medical history, mental illness history, social history, and current symptoms. Care providers use this information to develop a comprehensive treatment plan to address all of an individual’s problems and needs, including a co-occurring mental disorder.
According to the National Council on Alcoholism and Drug Dependence, Incorporated, “Research has consistently and clearly demonstrated the active involvement in self-help support groups significantly improves a person’s chances of long-term recovery”. An estimated 5 million people in the United States participated in some type of support group, including 12-step groups.

Dual Diagnosis Treatment
Treatment plans are highly individualized and address a person’s specific needs and issues. During dual diagnosis rehab, a variety of therapies are used to provide a whole-person approach to treatment that treats issues of body, mind and spirit for holistic healing.
Integrated treatment offers the best possible outcomes for a dual diagnosis, according to the Substance Abuse and Mental Health Services Administration, including:
- A reduction in substance abuse
- Improved mental illness symptoms
- Better cognitive functioning
- Reduced hospitalization
- Improved stability in a client’s home life
- Fewer legal problems
- A higher quality of life overall
Treating a dual diagnosis is a collaboration among treatment teams and involves:
- A single program that treats both disorders
- The same care providers treating both disorders
- An emphasis on a long-term recovery perspective
- Around-the-clock support
- Medications that may be used to treat one or both disorders
- An emphasis on developing a trusting relationship between the client and his or her providers
Both traditional and complementary therapies, administered in both group and individual settings, are used to treat a dual diagnosis. Traditional “talk” therapies include cognitive-behavioral therapy, dialectical behavior therapy, and family therapy. Complementary therapies include art therapy and mindfulness meditation. Medication may be used to treat symptoms of mental illness or to reduce cravings and normalize brain function. (This is known as medication-assisted treatment.)
Through therapy, individuals in dual diagnosis treatment:
- Learn strategies for coping with symptoms of mental illness
- Work through a variety of issues that contribute to the substance abuse
- Develop skills and strategies for coping with relapse triggers like stress and negative emotions
- Identify self-destructive patterns of thought and behavior and replace them with healthier ways of thinking and behaving
- Find purpose and meaning in a life without drugs or alcohol
- Learn to relax and have fun without substance abuse
- Repair damaged relationships
- Restore function to all of life’s domains
A variety of other services and interventions are used in treatment to address an individuals specific needs, including:
- Housing assistance
- Medical care
- Vocational rehab
- Educational assistance
- Financial counseling
- Life skills classes
- Parenting help
Dual Diagnosis Treatment Works
Hope is the foundation of recovery, according to the Substance Abuse and Mental Health Services Administration. Hope is the belief that a better life is possible, and this belief drives motivation and commitment in recovery. Through treatment, you’ll improve your life on many fronts and regain your sense of self-confidence, happiness, health and wellbeing for a brighter future for the long-haul.

 Matthew Beck B.A, M.A, LMFT
Matthew Beck B.A, M.A, LMFT 


