Meloxicam Addiction and Treatment
What is Meloxicam?
NSAIDs
Meloxicam is included under the class of drugs known as Nonsteroidal Anti-inflammatory Drugs or NSAIDs. These drugs are used to treat pain caused by inflammation. Some well-known over-the-counter (OTC) NSAIDs include ibuprofen (Advil), naproxen (Aleve), celecoxib (Celebrex), and aspirin. All of these medications work by lowering levels of prostaglandin, a hormone-like substance in the body that causes inflammation. While many NSAIDs can now be purchased OTC, meloxicam is available by prescription only.
Opioid Alternative
Meloxicam is a stronger NSAID developed and prescribed to offer an alternative to opioid drugs pain relievers. Because it’s more potent than other NSAIDs, it is prescribed at lower doses. It’s currently approved by the United States Food and Drug Administration (FDA) for the treatment of osteoarthritis, rheumatoid arthritis, and juvenile idiopathic arthritis. Researchers are also conducting clinical trials to determine the effectiveness of an intravenous solutions in the treatment of post-operative pain.2
Is Meloxicam a Controlled Substance?
The short answer is no. Meloxicam, like other NSAIDs, has been determined to have a low risk of addiction by the United States Department of Justice’s Drug Enforcement Agency (DEA). Only drugs that have a high risk of addiction are identified as controlled substances and placed on the controlled substances schedules specified by the Controlled Substances Act. Meloxicam is not one of these drugs and is not included on any controlled substances schedule.
Is Meloxicam Addictive?
Because it functions in a different way than opioids, it is not addictive. It also does not give a feeling of euphoria or “high,” as opioids and narcotics do.
That being said, it is possible to become dependent on meloxicam for pain relief. People who live with chronic pain, like that caused by various forms of arthritis, may rely on medications like meloxicam rather than implementing lifestyle changes that can help reduce pain.
People who rely solely on medications for pain relief tend to develop a psychological dependence on them, so a person who takes meloxicam for a chronic pain condition may perceive that they can’t function without the medication and may become anxious if they run out. This doesn’t mean that they don’t need the medication to relieve pain and improve function, but that they think that the medication is the only thing that will help them and that they have to have it no matter what.
Meloxicam Abuse
People who abuse meloxicam do not use it to “get high” because the drug will not work for this purpose. Many still use meloxicam as a pain reliever, just as it is intended, but they use it without a prescription and for purposes other than the treatment of arthritis. People who abuse meloxicam tend to abuse other drugs. Meloxicam may be used to relieve the side effects of other drugs, such as relieving the pain of a hangover after an alcohol binge or the side effects of an opioid as it begins to wear off.
Other people use meloxicam as a pain reliever, but they may take more of the medication than has been prescribed or may take someone else’s prescription for the drug in the belief that, since it is a supposedly safe pain reliever, it will relieve whatever pain they may have. In fact, research designed to measure patterns of NSAID use have found that people are often unaware of the potentially harmful side effects of NSAIDS and that they frequently take both OTC and prescription NSAIDs together, using higher doses than are recommended for those medications.
Side Effects of Meloxicam
The side effects that affect the stomach are quite common with meloxicam and may be more severe in children.
More serious side effects of meloxicam include:
Serious side effects require medical attention immediately. Anyone who experiences these serious side effects of meloxicam should contact their physician.
Interactions
It is important to remember that meloxicam may interact with other medications that people may also abuse, including:
- Anti-depressants
- Anti-anxiety medications
- Corticosteroids
- Lithium
Abusing meloxicam, along with these other medications, will further increase the risk of severe side effects and long-term health problems. It may also reduce the effectiveness of the other medications, even if they are taken as directed. And for someone already wondering, “do I have anxiety?”, this kind of misuse can make it even harder to understand what symptoms are caused by anxiety and what symptoms are triggered by the medications themselves.
2012 Case Study
A 2012 case study found that a woman who had been taking lithium for bipolar disorder with no problems developed lithium toxicity 3 days after beginning a daily dose of 15mg of meloxicam. The woman required a long hospital stay to resolve the toxicity. Healthy volunteers who were given meloxicam and lithium at the same time experienced an average increase in lithium concentrations of 21%.5
Be Brave. Get Help.
Long-Term Use of Meloxicam
Peptic Ulcer
The most common serious side effect of NSAIDs use is peptic ulcer, usually located in the upper gastrointestinal (GI) tract. It is estimated that people who take NSAIDs for chronic medical conditions have a relative risk of developing peptic ulcers up to 4.7 times higher than people who don’t use NSAIDs, and the hospital admission rate for GI tract conditions in people who use NSAIDs is estimated to be 121.9 per 100,000.
Risk Factors for Peptic Ulcer
The risk of peptic ulcers and other GI conditions increases with age, especially in people aged 65 and over. Other risk factors include a history of peptic ulcers, heart disease, and the use of multiple prescriptions, including corticosteroids and blood thinners, as well as the use of higher doses of NSAIDS.
In people who have multiple risk factors, the potential for the development of peptic ulcers increases to 9%. Out of all the NSAIDs, meloxicam is estimated to have intermediate-risk factors for the development of upper GI complications, at 2-4. Overall, this means the longer a person takes meloxicam, or the higher the dose of meloxicam, the greater the risk of developing peptic ulcers or other GI conditions.
Adverse Complications of Meloxicam
Although most serious side effects are associated with long-term use, even short-term use can increase the risk of developing adverse complications. The following chart shows the risk for the development of upper GI complications, myocardial infarction, and acute renal failure, based on the number of days NSAID therapy has been in place:
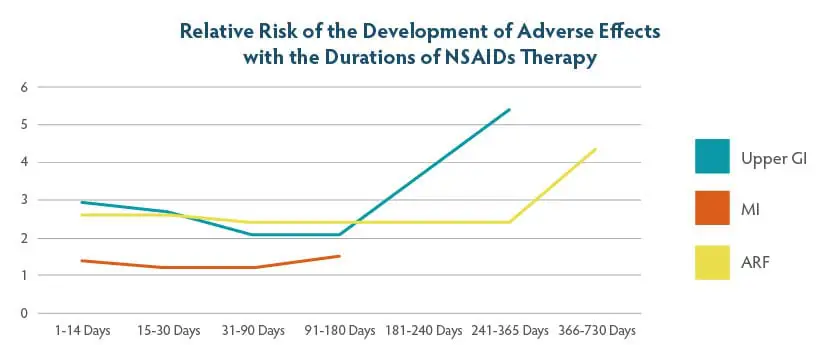
These numbers show that serious complications can occur even when NSAIDs are used for less than a year. Note the sudden increase in adverse effects after 180 days of use, reinforcing the fact that the longer NSAIDs are used, the higher the risk of serious adverse effects.
Meloxicam Overdose and Withdrawal
- Nausea
- Vomiting
- Drowsiness
- Fever
- Dizziness
- Fainting
- Black or bloody stools
- Coughing up blood
- Shallow breathing
- Infrequent urination or no urination
- Seizures
- Coma
These symptoms may be worse or may take effect faster if meloxicam is taken with alcohol. People who take prescription meloxicam should avoid alcohol even if they take the medication at the prescribed dose, as taking meloxicam with alcohol can aggravate gastrointestinal symptoms.
Does Stopping Meloxicam Cause Withdrawal?
Meloxicam is not an addictive substance, and, as stated before, it does not act on the body in the same way as opioids or other narcotics. Meloxicam does not cause withdrawal symptoms, and the drug does not have to be stopped by gradually lowering the dose. People who take meloxicam should follow the advice of their physicians when stopping meloxicam and switching to other pain relief therapies.
Problems with Mixing Substances
If a person takes meloxicam with addictive substances, such as alcohol, they may experience more severe withdrawal symptoms from the addictive substance due to the addition of meloxicam. Meloxicam’s side effects can compound or intensify the side effects and withdrawal symptoms of the addictive drug, making the withdrawal process significantly more difficult. Anyone attempting to stop using a combination of drugs that includes meloxicam should not try to manage withdrawal symptoms alone at home, but instead seek professional medical support through a physician or a trusted substance abuse treatment in Orange County to ensure a safe and supervised recovery process.
Reach out to verify your insurance coverage for addiction treatment
Alternative Treatments for Chronic Pain
Eating certain foods and avoiding other foods can help to control inflammation that causes pain. Fruits, vegetables, whole grains, beans, nuts, and fish help to control and reduce levels of inflammation that cause pain. Processed foods, greasy or fatty foods, and sweets tend to increase inflammation and pain.
Moderate exercise helps to keep muscles, nerves, and circulation in good shape, allowing bodily fluids to flow properly and preventing inflammation. Even if pain prevents a person from participating in vigorous exercise or sports, activities like walking, gentle yoga, or water exercise can help to keep the body in shape.
Pain causes stress, and stress causes more pain. This vicious cycle can be broken by using relaxation techniques to reduce tension in the body, which helps to reduce pain.
If pain becomes severe, or if painful conditions flare-up, a course of physical therapy may help to control the pain again. Physical therapists use agents such as heat, cold, or electronic treatments to reduce inflammation and increase blood flow in painful areas. This, combined with specific exercises, can help to reduce pain.
Chronic pain often leads to depression, anxiety, and stress. Cognitive-behavioral therapy teaches alternative ways of thinking about pain and alternative methods of coping with pain, helping to alleviate depression and anxiety.
Conclusion
Anyone who abuses meloxicam, whether to counteract recreational drugs or to control severe pain, should stop using this drug and should seek medical help immediately. Once these issues are resolved, our facility can help you overcome meloxicam abuse. Contact us today to learn more about our services.
Bekker, Alex; Kloepping, Carolyn; and Collingwood, Shemille. “Meloxicam in the Management of Post-Operative Pain: Narrative Review,” Journal of Anaesthesiology, Clinical Pharmacology, Medknow Publications & Media Pvt Ltd, 2018
Godersky, Margo E; Vercammen, Laura K; Ventura, Alicia S; Walley, Alexander Y; and Saitz, Richard. “Identification of Non-Steroidal Anti-Inflammatory Drug Use Disorder: A Case Report,” Addictive Behaviors, U.S. National Library of Medicine, July 2017.
Drini, Musa. “Peptic Ulcer Disease and Non-Steroidal Anti-Inflammatory Drugs,” Australian Prescriber, NPS MedicineWise, June 2017.

 Matthew Beck B.A, M.A, LMFT
Matthew Beck B.A, M.A, LMFT 


